THE INNOVATOR: Startup Of The Week: SPARK Microgravity
Meet the startup who won #1 EU Deep Tech Award 2025

Our best lab models for cancer often fail to predict clinical success. Microgravity offers a powerful complementary tool to bridge the gap between preclinical data and patient outcomes.
The Translation Gap
Traditional 2D cell cultures and animal models struggle to replicate the complex 3D architecture, microenvironment, and human-specific biology of tumors, leading to high failure rates in clinical trials1,2. More than 90% of oncology drug candidates that look promising in preclinical tests fail to translate into effective human treatments3.
A Complementary Bridge
Microgravity is not a replacement for these models but a crucial bridge. In the near-weightless environment of space, cancer cells grow as 3D multicellular spheroids that closely mimic human tumors – capturing native cell-to-cell interactions, oxygen/nutrient gradients, and architectural complexity that flat Petri dishes cannot4,5. This yields more human-relevant, predictive data on drug responses.
Strategic Integration
Orbital research can be strategically integrated into the R&D pipeline at key decision points. For example, microgravity experiments can evaluate a drug’s efficacy on realistic tumor spheroids or elucidate its mechanism of action in a human-like tumor-immune co-culture, before committing to costly late-stage trials6. In essence, space becomes an in vitro testing ground for how a therapy will perform under human-like conditions of growth and stress.
De-Risk Your Pipeline
By providing a clearer preview of how a compound will behave in a human-like 3D system, microgravity studies help “de-risk” oncology programs. Promising activity observed in microgravity-built models can give confidence to advance a drug, while a lack of efficacy or unexpected toxicity in these more realistic models can save resources by signaling failures early7,8. The result is a more efficient path to viable therapies with fewer late-stage surprises.
For nearly a century, the petri dish has been the workhorse of cancer research. Growing cancer cells in a flat, two-dimensional monolayer is inexpensive and high-throughput. However, this simplicity comes at a cost: a 2D culture is an artificial environment that fails to capture the complexity of a real tumor9,10.
A tumor in the human body is a three-dimensional structure with intricate architecture, varied oxygen and nutrient levels, and complex mechanical forces. They experience unnaturally uniform nutrient and oxygen availability and are subject to the high stiffness of the plastic substrate, which is far from the softer extracellular matrix of a living organ11,12. These differences profoundly affect cell behavior: tumor cells in 2D spread into a flattened shape and respond to mechanical cues that differ from those in a 3D tissue13.They lack the cell-to-cell and cell-to-matrix interactions that drive tumor growth, invasion, and drug resistance.
As a result, cells in 2D culture proliferate and respond to drugs in ways that often do not predict their behavior in vivo14,15.
It is a fundamental mismatch – a drug that efficiently kills cancer cells on a plastic dish often has little to no effect on a solid tumor in a patient, because the dish cannot replicate the tumor’s microenvironment and heterogeneity1617.
In short, two-dimensional models, while useful for basic screening, oversimplify tumor biology and can give false confidence about a therapy’s potential18,19.This fundamental mismatch is why a drug that effectively kills cancer cells in a dish often has little to no effect on a solid tumor in a patient.
To overcome the limitations of 2D cultures, researchers turn to animal models, most commonly mice. These models allow scientists to study tumors within a living system, complete with a blood supply and an immune system. While invaluable, animal models have their own significant drawbacks that contribute to the translational gap.
The mouse immune system is not the same as the human immune system. This is a critical issue for evaluating immunotherapies, which are designed to work specifically with human immune cells and proteins.
Mice and humans vary in immune cell types, protein receptors, and cytokine networks, meaning that an immunotherapy which engages human T-cells or checkpoint proteins may not function properly in a normal mouse20. T
raditional mouse tumor models often use either fully murine immune systems (syngeneic models) or severely immunodeficient mice to grow human tumors (xenografts). Neither is ideal for testing modern immunotherapies: a syngeneic mouse’s immune checkpoints differ from a human’s, while an immunodeficient mouse lacks the functional human immune components altogether21. Indeed, it’s now recognized that humanized mouse models (mice engrafted with human immune cells) are needed to more faithfully evaluate immunotherapies22,23. Without a human-like immune context, animal studies can misrepresent how checkpoint inhibitors, cancer vaccines, or cell therapies will perform in patients.
Mice metabolize drugs differently than humans due to species-specific differences in physiology and enzyme function24,25.
A compound that is safe and effective in a mouse at a given dose may be toxic or ineffective in a person.
For example, metabolic rate differences (mice have a much faster metabolism) and variations in liver enzymes can lead to discrepancies in drug clearance and bioavailability26. There have been notable cases where a therapy showed no adverse effects in animal tests but caused severe toxicity in humans – a stark reminder that animal physiology can mask dangers that only appear in human biology27. Conversely, some drugs fail in mice due to rodent-specific sensitivities yet could have worked in humans. These pharmacokinetic and pharmacodynamic mismatches mean that animal results do not always translate to the clinic.
Mouse tumors generally grow much faster than human tumors, often forming aggressive masses within weeks. This rapid timescale fails to capture the prolonged evolutionary dynamics of human cancers, which develop and diversify over years. Human tumors typically exhibit extensive genetic heterogeneity and subclonal evolution; a patient’s cancer might contain multiple populations of cells with different mutations. Mouse models (especially transplanted cell lines) often lack this diversity or favor a dominant clone, and they usually do not reflect the gradual acquisition of resistance mechanisms that occurs in patients30,31. Additionally, many mouse models use young, inbred mice kept in controlled laboratory conditions – starkly different from the heterogeneous genetic background and environmental influences present in human patients. These differences in tumor biology and host context help explain why results from mouse studies so often fail to predict what happens in human clinical trials32. The animal model is an approximation; for many modern targeted therapies or immunotherapies, that approximation isn’t close enough to mirror human reality.
These differences explain why results from animal studies so often fail to predict what will happen in human clinical trials. The model is an approximation, but for many modern, targeted therapies, that approximation isn't close enough.
These disconnects between preclinical models (both cell culture and animal) and human reality create what is known as the “translation gap.”
Promising results in the lab too often do not lead to success in the clinic. In fact, over 90% of oncology drugs that enter clinical trials after showing efficacy in preclinical studies end up failing in human trials33,34. This staggering failure rate – on the order of only about 10–15% success or less – is well documented across the pharmaceutical industry. Analysis of drug development pipelines shows an overall failure rate above 90%, with late-phase efficacy failures being especially common in oncology35,36.
The cost of these failures is enormous. Every drug that reaches human trials represents years of work and an investment in the hundreds of millions of dollars. When 9 out of 10 such candidates fail, it results in billions in sunk R&D costs37. More importantly, it delays the delivery of effective new treatments to patients who desperately need them. For cancer patients, each failed trial is a lost opportunity and more time without better therapy options.
The core problem underlying this attrition is a lack of predictive power in our traditional preclinical models38.
Simply put, 2D cell assays and mouse models are not giving us an accurate enough preview of how a drug will perform in the complex, dynamic environment of a human patient. They can over-predict efficacy (drugs look like “cures” in mice but do little in people) and under-predict toxicity (safety issues emerge in humans that weren’t evident in animal studies). This disconnect means that by the time a drug reaches Phase II or Phase III trials – the first points at which we truly see human efficacy – a huge amount of time and money has already been spent on a candidate that may flop. The translation gap thus acts as a sieve, with only a small fraction of initial “hits” making it through to become approved treatments39.
To close this gap, we do not necessarily need to replace our current tools, but we do need to augment them with better, more human-relevant models. The ideal scenario is to identify likely failures before they reach costly clinical trials, and to identify the most promising drug candidates sooner with greater confidence. This is where emerging technologies come in – from organ-on-a-chip systems to advanced 3D cultures and patient-derived organoids. Among these, an unexpected but powerful approach has entered the scene: using microgravity, the condition of near weightlessness experienced in space, to grow more physiologically relevant cancer models40,41.
Microgravity research offers a transformative middle ground between simplistic lab models and complex human biology.
By taking cancer cells to low Earth orbit (or by simulating microgravity on Earth), scientists can create 3D tumor models that more closely resemble those inside patients42,43. In the absence of strong gravity, cultured cells no longer settle into a flat layer; instead, they tend to aggregate and grow in three dimensions. Cancer cells in microgravity float and self-assemble into multicellular spheroids, adopting structures akin to tumor nodules44,45. These spheroids recapitulate many features of real tumors: cells on the outside and interior experience different levels of oxygen and nutrients (creating gradients and even hypoxic cores), and they establish cell-to-cell contacts and produce extracellular matrix, developing architecture that mirrors in vivo tumors46,47.
Notably, microgravity allows tumor cells to grow without the need for artificial scaffolds – the cells’ own interactions are enough to form a tissue-like assembly48. Studies have shown that microgravity conditions can improve nutrient and waste exchange in 3D cultures, preventing the diffusion limitations that often plague large spheroids on Earth49. The result is often larger, more uniformly grown tumor spheroids that can be maintained for extended periods. For example, researchers have observed that aggressive cancer cells sent to the International Space Station (ISS) formed spheroids that tripled in size in just 10 days, demonstrating how microgravity facilitates rapid 3D growth50,51. These structures are not just blobs of cells – they are organized in ways that simulate how a tumor might grow and respond in a human body, including the development of drug resistance pockets or quiescent cell zones.
Microgravity thus acts as a unique kind of bioreactor, one that coaxingly pushes cancer cells to reveal their true nature. It provides a cleaner, more relevant context to study fundamental cancer biology and drug responses. Importantly, this approach is complementary: it is not meant to replace animal models or other in vitro systems, but to fill an important gap between them52,53. A microgravity-grown tumor spheroid is more complex and human-like than a 2D culture, yet it avoids some of the species differences and complexities of whole-animal models. In essence, it’s a bridge model – more predictive than a petri dish, and used as an intermediate step before moving into expensive animal studies or clinical trials54,55.
The potential of this approach is increasingly recognized. Researchers around the world have begun conducting cancer experiments in orbit, and the results have been striking56,57. Tumor cells grown in microgravity have shown changes in gene expression and behavior that provide new insights into cancer aggressiveness and treatment sensitivity58,59. Even phenomena like cancer stem cell formation, invasion, and metastasis-related signaling can be studied in these 3D aggregates formed off-Earth. For instance, one ISS study on a pediatric brain cancer (diffuse midline glioma) is using microgravity to investigate tumor biology that is hard to probe in animal models60. Another line of research involves crystallizing cancer-related proteins (like mutant KRAS) in microgravity to achieve higher resolution structures for drug targeting61,62 – something that directly leverages microgravity to improve drug design.
It must be emphasized that microgravity is not a magic bullet – it’s a tool to make models more human-like, thereby hopefully improving predictive power. By integrating this tool into the oncology R&D pipeline thoughtfully, companies can obtain data that better forecasts clinical results, helping to guide decision-making.
Integrating microgravity experiments into an oncology R&D pipeline is a strategic decision. The idea is to deploy this approach at high-leverage decision points – those moments when you need additional evidence to determine whether a drug candidate is worth further investment, or to deeply understand how it works. Rather than launching every experiment into space, R&D teams can select specific questions that microgravity is uniquely suited to answer63. Below we outline two sample workflows where orbital research could be utilized for maximal impact:
Sample Workflow 1: Early Efficacy Screening
Notably, one recent microgravity experiment found that a breast cancer organoid treated in space responded more quickly, with tumor growth reduced at a faster pace than on Earth under the same treatment64. Such results de-risk the decision to move into animal studies or early-phase trials. Conversely, if the drug performs poorly – e.g. minimal growth inhibition of spheroids – it can trigger an early no-go decision, saving the company the expense of further development. In this way, microgravity efficacy screening acts as a filter to weed out candidates that might falter in clinical conditions, sparing resources and time.
Sample Workflow 2: Mechanism of Action Studies
While powerful, microgravity is not a silver bullet. It’s essential to understand its limitations and the aspects of drug development it cannot fully replicate. An orbital lab cannot simulate the full systemic complexity of a living patient – for example, long-term drug metabolism by the liver, interactions with endocrine and neurological systems, or the psychology of patient adherence! Some specific limitations include:
For this reason, microgravity research should be seen as one component of a broader evidence-gathering strategy. Promising results from orbital experiments should be validated with data from orthogonal models, including advanced terrestrial 3D cultures and, where appropriate, carefully designed animal studies. The goal is to build a comprehensive, multi-faceted case for a drug's potential before entering human trials.
Oncology R&D faces a clear challenge: we need more predictive models to close the gap between the lab bench and the clinic.
Patients’ tumors are incredibly complex, and our traditional testing methods often fall short of capturing that complexity. The consequence has been a costly drag on development, with too many failures late in the game. Microgravity provides a unique and powerful way to change this. It offers a window into cancer behavior under conditions that foster human-like tumor architecture and cell interplay65,66. By strategically integrating orbital research into drug development, we can make smarter decisions earlier. We can identify false leads before they consume vast resources, and we can recognize true winners with greater certainty thanks to more lifelike efficacy signals. In doing so, we de-risk the pipeline: fewer surprises in Phase III, more line-of-sight between preclinical promise and clinical success67.
Microgravity research is not science fiction or a distant future idea – it is happening now. Pharma companies have already sent experiments to space to benefit their programs. For example, Amgen used ISS flights to test osteoporosis drugs in microgravity, which helped strengthen their FDA approval packages68. Merck sent Keytruda (an antibody for cancer) to space to explore new formulations69. Startups are emerging with the explicit goal of leveraging microgravity for drug discovery, effectively turning space into a service for biotech70,71. All this points to a new paradigm: space-enabled biotech as a part of mainstream R&D. What was once an experimental oddity is becoming a practical tool.
For R&D leaders, the message is that microgravity can be woven into the fabric of your innovation strategy.
It requires adjusting to new logistics and collaborations (partnering with space organizations or specialist vendors), but the payoff is accessing an extraordinary experimental condition that was never before available. As the ecosystem grows – with commercial space stations on the horizon and dedicated microgravity research services – the accessibility will only improve. Those who start building microgravity into their pipeline now will define the learning curve for everyone else.
Ultimately, the mission is to build a better bridge from lab to clinic. Every new model or method that improves predictiveness is a pillar in that bridge. Microgravity stands out as an especially intriguing pillar – one that brings us closer to mimicking the patient’s reality before we ever enter a patient. By reducing the translational uncertainty, we increase the odds of success, cut down development timelines, and most importantly, deliver effective therapies to patients faster and with greater confidence.
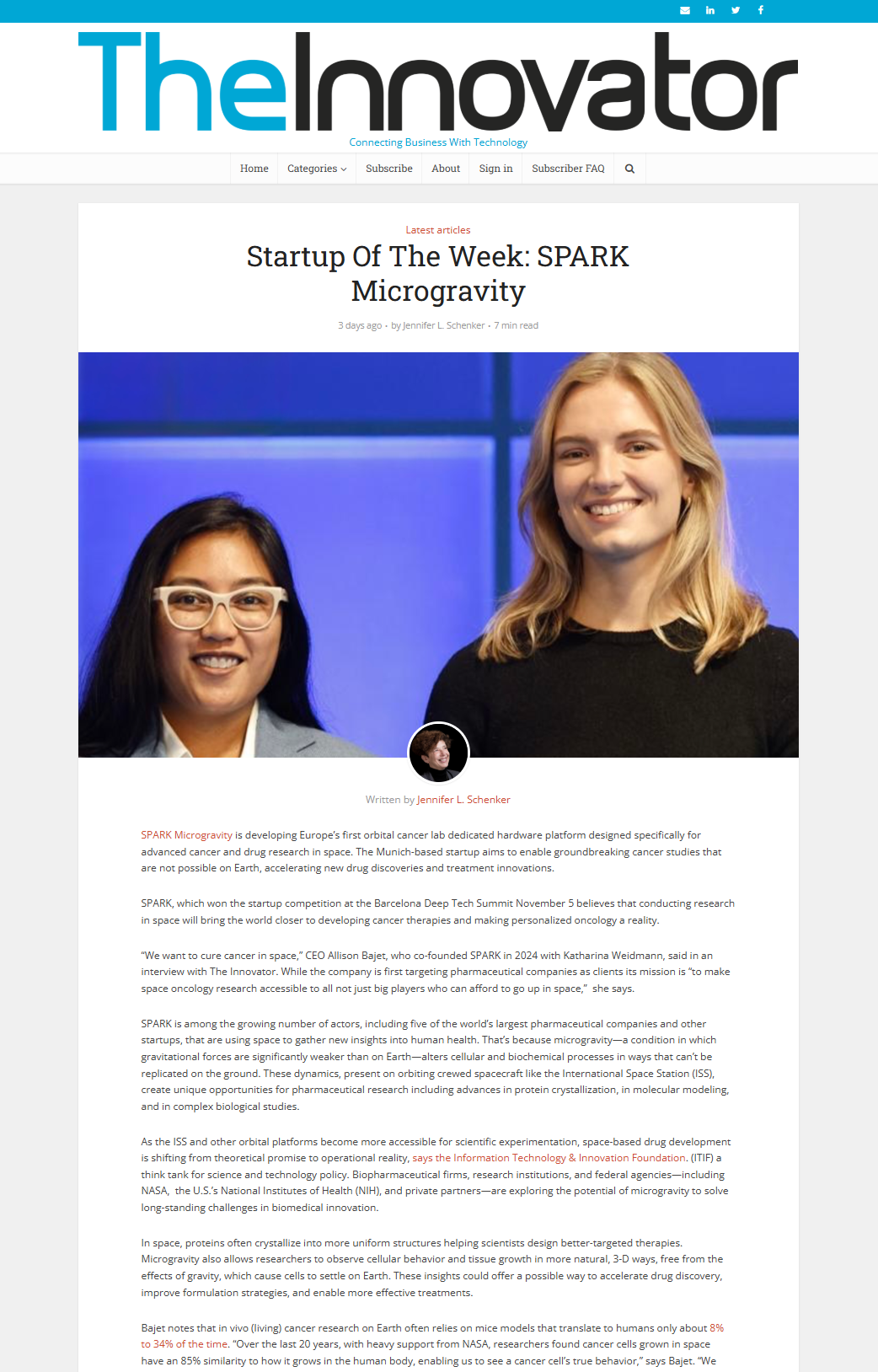
SPARK Microgravity is a startup dedicated to democratizing space research and making it accessible for researchers across the globe. Headquartered in Munich with operations in the U.S. and Europe, SPARK Microgravity is building Europe’s first orbital cancer research laboratory to accelerate oncology breakthroughs in microgravity. By providing end-to-end microgravity research services – from experiment design and launch integration to data analysis, SPARK Microgravity enables pharmaceutical companies to leverage the space environment for R&D. Our mission is to advance scientific exploration in low Earth orbit and translate those discoveries into life-saving innovations back on Earth.
Meet the startup who won #1 EU Deep Tech Award 2025

SPARK Microgravity's co-founders share their space research mission during an interview at Barcelona Deep Tech Week 2025.
.svg)